The Top Five Fruits That Can Help Prevent Diabetes
Diabetes is a disease that can be brought about by a person’s lifestyle and environment. Diabetes is caused when the pancreas cannot produce enough insulin or the body cannot use
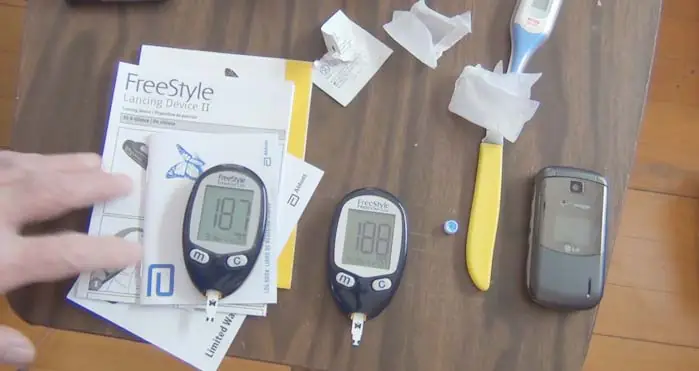
The Best Way to Reuse Diabetic Test Strips
Diabetic test strips help diabetics measure their blood sugar and can be purchased in boxes of 100. Most people just throw away their used test strips, but there are multiple
Insulin Burn: What Causes It and Why it’s Uncomfortable?
Some of the most common reasons for high blood sugar are a diet that’s high in sugar, and lack of physical activity. When your body doesn’t produce enough insulin to
How to Clean the Memory of the Freestyle Lite Glucose Meter?
The Freestyle Lite glucose meter is an affordable and convenient way to keep track of your health. The meter tests for glucose levels with a simple finger prick that lasts
Readings of Different Blood Sugars on Different Fingers
Dealing with a diabetes diagnosis can be difficult. It’s important to remember the finger-pricking technique when you are taking your blood sugar readings so you know what your results mean.
Diabetes and Insulin: A Guide to Taking Insulin the Right Way
Diabetes is a disorder that can cause serious health problems. Properly taking insulin can be the difference between improved health and worsening diabetic symptoms. This article will provide tips for
Is Sushi A Good Choice For Those With Diabetes?
Sushi is a diabetics friendly food. Sushi has low sugar, and the sugar doesn’t spike like other foods do. The type of sugar in sushi is natural sugar. It’s super
What is the Process Of Clearing The Memory On A Glucometer?
A glucometer is a tool or device that is used for measuring the concentration of glucose. There are two types of measurements mg/dL and mmol/L. One of the methods of
Living With Diabetes: How To Deal With The Daily Challenges
My daughter was diagnosed with diabetes just a short while ago. It has been very difficult for her and it’s also been a big change for our family. Many days,
What Is The Cause Of Heart Pain After Eating Sugar?
Sugar is not only a treat for the taste buds but also an ailment for the heart. When we consume sugar, our body produces insulin to help digest it. This
10 Brilliant Examples of AI in Marketing
10 Key Uses of Artificial Intelligence in Marketing: Examples However, email marketing is more complicated than drafting copy and hitting send. The most effective email marketing campaigns are carefully segmented,

 1-772-212-0292
1-772-212-0292